De jaarlijkse Staat van Zoönosen focust zich dit jaar op een One Health-aanpak van zoönosen. De One Health-gedachte gaat er vanuit dat verschillende disciplines moeten samenwerken bij de aanpak van zoönosen. Deze samenwerking is nodig, omdat mensen en dieren in relatie staan met elkaar en hun omgeving.
De Staat van Zoönosen, een gezamenlijke uitgave van het RIVM en verschillende partners, verschijnt jaarlijks en biedt een overzicht van de meest belangrijke ontwikkelingen en trends op het gebied van zoönosen (ziekten die van dier op mens kunnen overgaan). Het is belangrijk om inzicht te hebben in de ontwikkeling van deze ziekten, zodat tijdig gehandeld kan worden als dat nodig is.
Vooral bacteriële voedselinfecties
De meeste infecties van dieren naar mensen worden via voedsel overgedragen. In 2017 zijn in totaal 666 uitbraken gemeld van voedselgerelateerde uitbraken met 2995 zieken. Een deel hiervan werd veroorzaakt door zoönotische voedselgerelateerde ziekteverwekkers, zoals Campylobacter, Salmonella, Listeria monocytogenes en STEC. Voor listeriose valt een toename van het aantal patiënten over de jaren op.
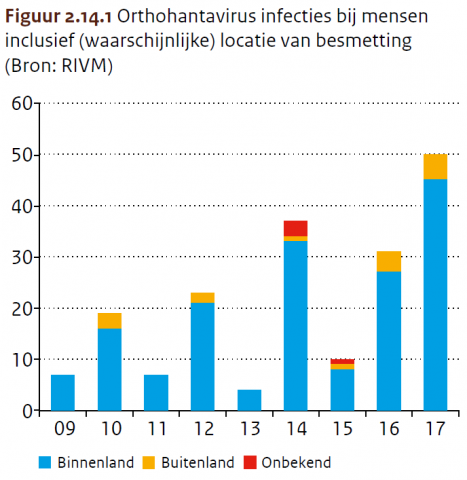
Meer patiënten met orthohantavirus-infectie
Orthohantavirussen komen voor in knaagdieren, zoals rosse woelmuizen en ratten. In Nederland komen puumalavirus en, sinds 2016, seoulvirus het meeste voor. Besmette knaagdieren kunnen het virus uitscheiden in hun urine of ontlasting. Als dit indroogt, kan het virus in stof terechtkomen, waarna mensen het kunnen inademen. Dit kan leiden tot griepachtige klachten en nier- of leverklachten. In 2017 zijn 50 personen gemeld met een orthohantavirus-infectie (waarvan 45 opgelopen in Nederland). Net zoals in 2016 waren er ook in 2017 een aantal patiënten besmet geraakt met seoulvirus via tamme ratten (3 in 2017).
Verdere daling leptospirose, maar nog steeds hoog
Al enige jaren is het aantal patiënten met leptospirose hoog. In 2017 waren er 71 patiënten met leptospirose. Dat is iets minder dan in 2015 en 2016 (89 en 84), maar nog steeds veel hoger dan de jaren ervoor. In 2017 had de meerderheid van de patiënten de ziekte opgelopen in het buitenland. De bacteriën zitten in de urine van ratten en muizen. Vooral via zwemwater en modder raken mensen besmet. De verschijnselen van leptospirose bij mensen verschillen van milde griepachtige verschijnselen tot een ernstig ziektebeeld met geelzucht, nierfalen en bloedingen (ziekte van Weil).
Meer gevallen van Brucella in honden, niet in mensen
Eind 2016 werden voor het eerst Brucella canis besmettingen bij 4 honden in Nederland geconstateerd. In 2017 werd de bacterie bij 13 honden aangetoond. Het betrof in alle gevallen honden die geïmporteerd waren uit Zuidoost-Europa. In Nederland zijn voor zover bekend geen mensen ziek geworden van de Brucella-bacterie.