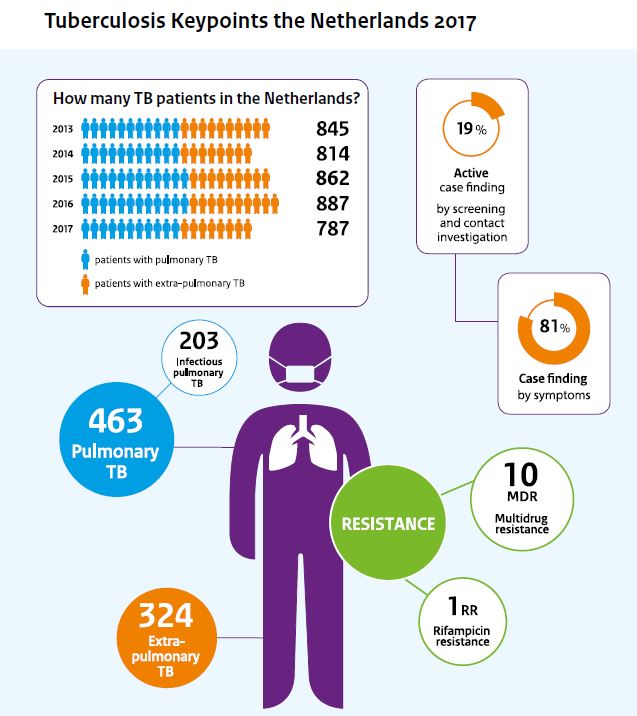
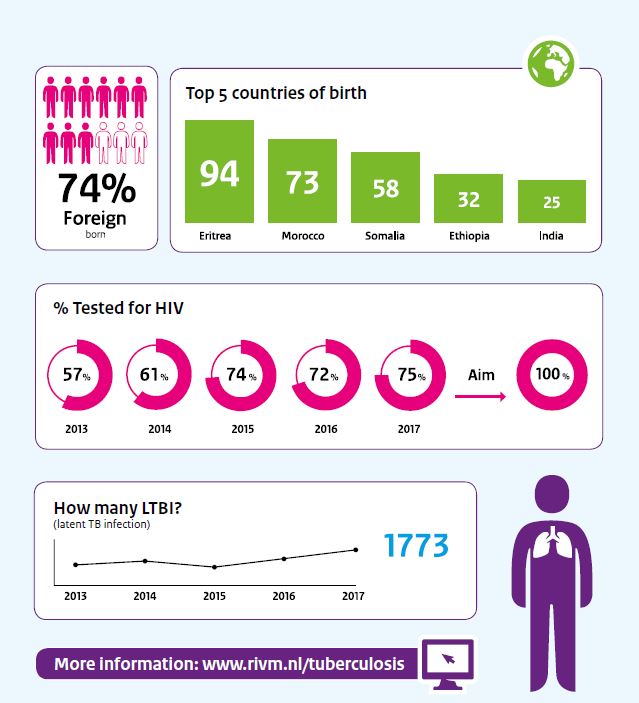
The number of tuberculosis (TB) patients in the Netherlands decreased considerably in 2017. From 887 patients in 2016 to 787 in 2017. Nearly three-quarters of the TB patients in the Netherlands are born in countries where TB is still very common, such as Eritrea, Morocco and Somalia. This is published by RIVM in the annual tuberculosis report 2017. Various factors led to the decline, such as a decreasing number of immigrants and asylum seekers in 2016 and 2017, as well as the falling incidence of tuberculosis in the Dutch population.
Tuberculosis is caused by a bacterium. Tuberculosis can be contagious, for example, if the disease is located in the lungs. Its most infectious form (open tuberculosis) was observed in a quarter of patients in 2017. RIVM reports these figures annually in order to monitor the progress of measures for tackling tuberculosis in the Netherlands.
Screening
Cases are notified to the Municipal Public Health Services. Most patients (eighty per cent) went to the doctor of their own accord; ten per cent were found by screening high-risk groups and eight per cent by examining people after exposure to infectious patients (contact tracing).
Tuberculosis and HIV
HIV infection increases the risk of tuberculosis. It is important to identify and treat an HIV infection as early as possible. TB patients in the Netherlands are therefore offered an HIV test. The percentage of TB patients in the Netherlands who have been tested for HIV rose from 28 per cent in 2008 to 75 per cent in 2017. In 2017, 23 TB patients were infected with HIV.
Complete treatment
For a successful treatment of tuberculosis, patients must take a number of medicines for six months or more. It is important that patients complete their treatment. The Dutch National Tuberculosis Control Plan has set the target that 90 per cent of TB patients should complete their treatment. This objective was achieved in 2016 for patients whose bacterium was not resistant against rifampicin, one of the key drugs to treat TB. The treatment results for 2017 are not known yet.
Resistance
When the TB bacterium is resistant for rifampicin, a complex and lengthier course of treatment is required. Over the last five years, the number of patients with rifampicin-resistance in the Netherlands varied between ten and twenty. There were eleven patients in 2017.