Mpox is a disease caused by the mpox virus. People with mpox get bumps or blisters (pox) that are painful and can leave scars. In the past, the disease was sometimes referred to as monkeypox.
What is mpox?
Mpox is a viral infection that originally occurred mainly in West and Central Africa. It is a zoonosis: a disease that can be transmitted from animals to humans. In Africa, the virus is mainly transmitted to humans from rodents, rabbits and monkeys. People can also transmit the virus to each other.
The mpox virus can be categorised into two main groups: Clade 1 and Clade 2. In 2022, there was a global outbreak of infections involving an mpox variant from Clade 2: mpox 2b. There was also an outbreak of mpox in the Netherlands, which mainly affected men who have sex with men.
Since 2023, there have been several outbreaks in Central Africa involving mpox viruses from Clade 1. In addition to the previously known mpox variant 1a, which is mainly transmitted from animals to humans, a new variant from Clade 1 was also found: mpox 1b. Mpox variant 1b can also spread through human-to-human transmission. However, much is still unclear about variant 1b.
For example, we do not know if this variant is more infectious than variant 2b, and whether there are differences in disease severity. There have only been a few infections involving this variant outside Africa, which makes it difficult to draw reliable conclusions. This is because the situation in Africa cannot easily be compared to the situation in Europe. So far, there do not seem to be very significant differences in contagiousness and disease severity. However, it is clear that both variants can be transmitted through direct contact with someone who has mpox.
What are the symptoms of mpox?
The main symptom of mpox is the skin rash. These pox can present as red spots, bumps or blisters. They can be painful. The blisters dry up and form a crust, leaving scabs that fall off 2 to 3 weeks later. They may cause permanent scars.
Other symptoms associated with mpox include:
- fever
- headache
- muscle ache
- swollen lymph nodes
- chills
- tiredness
Some cases of mpox start with these symptoms followed by the skin rash, while others start with the rash and then develop other symptoms. The pox can also occur in the mouth and form ulcers. During the 2022 outbreak, people regularly also had proctitis, a painful inflammation of the lining of the rectum (the final part of the intestines). Sometimes proctitis is the only symptom.
What does mpox look like?
Phase 1

Mpox on finger, phase 1
Phase 2

Mpox on finger, phase 2
Phase 3

Mpox on finger, phase 3
How does mpox spread?
Anyone can get mpox. The virus is transmitted through close or intimate contact (cuddling, kissing, making love and sexual intercourse) with someone who has mpox. Most reported cases of people with mpox in the Netherlands have involved MSM contact (men who have sex with men). The highest risk of infection is among men who frequently have sex with different male partners.
The blisters and the scabs from the blisters can transmit the virus. The virus can enter the body through the mucous membranes or through tiny wounds or tears in the skin. Very occasionally, the virus is also transmitted through contact with contaminated materials (such as bedding or towels). The virus may also be able to spread via droplets from the mouth and nose while talking or breathing, if people are very close to each other. The risk of spreading mpox in this way currently appears to be minimal.
Some people develop flu-like symptoms or a skin rash before the pox appear. They may already be contagious at that point. The pox may also form in less visible locations, such as in the mouth (ulcers) or inside the rectum. Some people with mpox only have 1 blister.
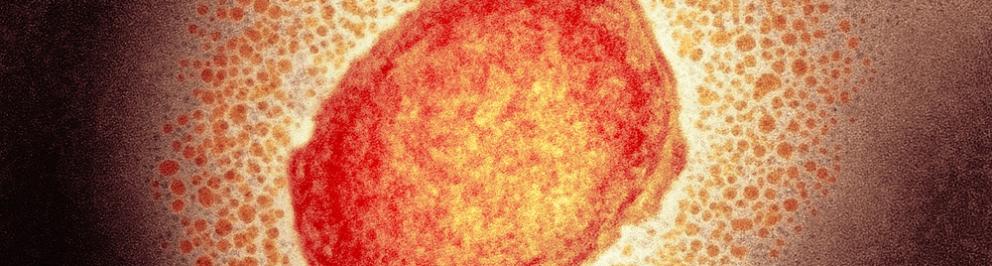
Close-up of an mpox lesion
How can I prevent mpox?
You can reduce the risk of mpox by not having intimate or skin-to-skin contact with people who have mpox. In regions with mpox outbreaks, it is important to be alert and avoid intimate contact and direct skin contact. Less contact involving sex and cuddling lowers the risk of infection.
By quickly recognising symptoms that could indicate mpox, you help prevent the virus from continuing to spread. If you or your partner may have been infected, it is important not to have sexual intercourse or any intimate contact – not even with a condom. If you or your partner has had mpox, the recommendation is to use a condom during sex for 5 weeks after the first pox appear.
From 14 April 2025 through at least the end of 2026, a vaccination against mpox is available from the Municipal Public Health Services (GGDs) for men who have sex with men (MSM) and transgender people. The aim is to prevent infections and outbreaks and to minimise the burden of disease.
What should I do if I have mpox?
- If any of the following apply, call your GP or the Municipal Public Health Services (GGDs):
You have 1 or more blisters or sores on your body, especially around the anus, penis or vagina or on the face, and you are a man who has sex with men. - You have 1 or more blisters or sores on your body, especially around the anus, penis or vagina or on the face, and you have been in a region of the African continent where mpox is currently prevalent (such as the Democratic Republic of Congo and the surrounding countries).
- You have had close contact or sexual contact in the past 3 weeks with someone who has mpox.
The GP or GGD may test you for mpox. If you test positive for mpox, the Municipal Public Health Service (GGD) starts source and contact tracing. The aim is to find out who gave you mpox and who in your surroundings may be at risk for getting mpox. Your contacts who have a high risk of getting mpox can be vaccinated in consultation with the GGD.
If you test positive for mpox, you need to self-isolate (stay at home) and follow the rules for self-isolating during mpox. You should not have any physical contact with others until all the symptoms are gone. In the context of mpox, that means that all the scabs from the blisters must have fallen off and new skin must have formed. This is because the scabs can also transmit the virus. It often takes 2 to 3 weeks for the scabs to go away. If you also have proctitis (inflammation of the lining of the rectum), all the symptoms associated with proctitis, such as anal discomfort, must also have resolved completely.
Is there any treatment for mpox?
In most cases, mpox goes away on its own within a few weeks. Sometimes a doctor recommends antiviral drugs.
How common is mpox in the Netherlands?
In 2022, a Clade 2 mpox virus was detected in people in Europe who had no direct connection to the affected areas in Africa where the disease has been circulating for some time. Mpox then spread throughout Europe, North America and other new areas. People in the Netherlands also contracted mpox. After a spike in the summer of 2022, the number of reported cases declined sharply in the fall of 2022. Mpox cases caused by variant 2b rose again in the Netherlands at the end of 2024.
In August 2024, the World Health Organisation (WHO) declared an international public health emergency in response to the mpox outbreak in the Democratic Republic of Congo (DRC) and surrounding area. Tens of thousands of suspected and confirmed infections and hundreds of deaths were reported. Some of these involved the mpox variant 1b. Since that time, infections involving the new mpox variant 1b have been confirmed in various European countries. These include the United Kingdom, Germany, Sweden and France. Most cases involved individuals returning from Africa.
In October 2025, infections involving mpox variant 1b were reported in Spain, Italy and Portugal among people without any travel history. A number of these people were men who have sex with men (MSM). There are now people with this mpox variant in the Netherlands. It is possible that there will be more cases. The risk that the virus will continue to spread among the general population is low.
RIVM is closely monitoring the reported cases of mpox and posting updates on the current situation in the Netherlands and internationally.