When you are infected with a virus, your body responds by producing antibodies. Your body also produces antibodies after vaccination. Antibodies recognise the virus and help your body fight it. The immune system in your body makes these antibodies.
Everyone has many different antibodies. Each of them recognises intruders, including various types of viruses and bacteria that can make us ill. The immune system has special cells (known as B cells) that make the antibodies. It takes time for your body’s immune system to recognise the pathogens that can make you ill. This could take a week, or sometimes as long as 3 weeks.
A virus or bacteria is much larger than an antibody. That is why it takes lots of antibodies working together to fight viruses and bacteria.
How an antibody responds to an infection
The coronavirus SARS-CoV-2 enters the body through our respiratory system (nose, mouth and airways). The virus clings to the walls of our airways. Then it penetrates into the cells of our body. When the virus enters into the cells, this is called an infection. An antibody that recognises the coronavirus will attach itself to the outside of the virus. Antibodies on the surface of the virus can prevent the virus from invading more cells. That stops the infection.
Figure: BioRender.com
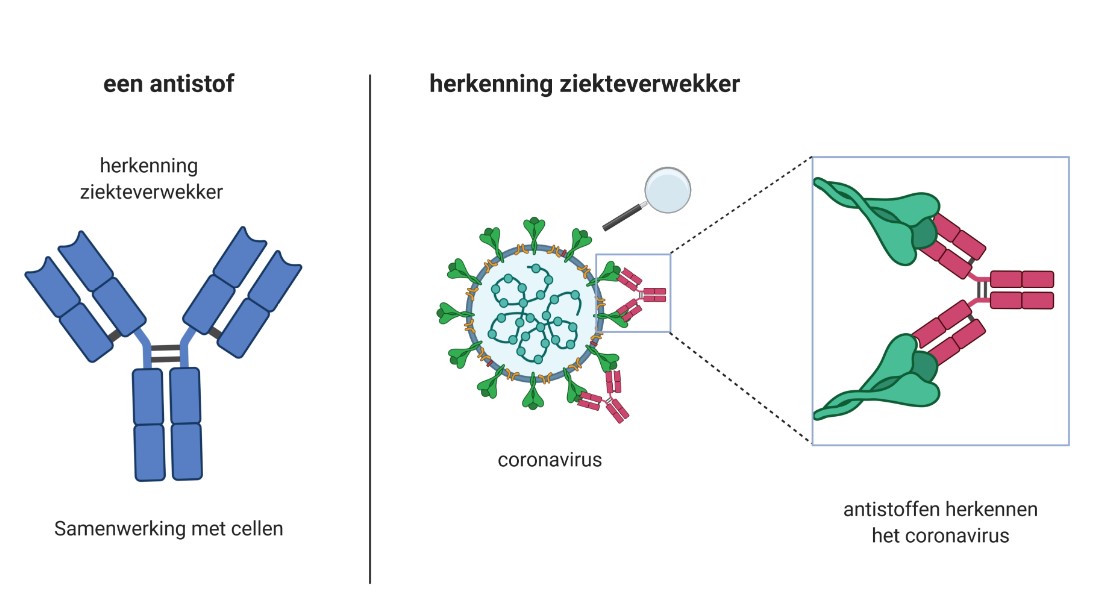
Left: antibody: pathogen recognition; interaction with other cells.
Right: recognising a pathogen; antibodies recognise the coronavirus.
Antibodies are often shown as Y-shaped. The two tips can recognise pathogens. That means that 1 antibody can recognise 2 pieces of the same pathogen at once. The trunk of the antibody interacts with the cells of the immune system, working with the B cells and other cells that clean up and destroy viruses. Because they work together, your body can clear the virus even more effectively.
What it means if you have antibodies
If you have antibodies in your blood but have not yet been vaccinated, that means that you were previously infected with the virus. When you are vaccinated, your body also makes antibodies. Once that happens, if you come into contact with the virus, you will be protected, for example by those antibodies. Research is being conducted to find out how high the antibody levels need to be to fully protect someone from the virus, and how long that protection lasts.
People who have not been infected with the virus and have not been vaccinated do not have any antibodies against the coronavirus SARS-CoV-2.
Your immune system remembers
When the B cells notice that the virus is back again, they can respond very quickly to make more antibodies. That response is part of how your immune system remembers the virus. The more antibodies you have, the more virus particles are recognised by your immune system, and the harder it is for the virus to invade your cells. In most people, this prevents them from becoming ill. Initial research results show that people who are infected after a previous infection or vaccination and therefore have antibodies have lower levels of the virus in their system.
How RIVM measures antibodies
RIVM has a test that measures antibodies. Antibodies are usually measured in a blood sample, and sometimes in a sample of mucus taken from your airways. The most important antibodies against the coronavirus are the antibodies that recognise the spike proteins. These spikes cover the exterior of the coronavirus. This makes the virus look like a crown (or corona in Latin). That is where the coronavirus gets its name.
In the laboratory, we take various proteins from the virus (including the spike protein) and attach them to tiny plastic balls, which are then added to the blood samples of people who take part in the studies looking at antibodies, such as the PIENTER Corona Study. These balls can be viewed using special equipment. If there are antibodies in the blood sample, they will cling to the tiny balls with the proteins from the virus. After the test, we will know if there are antibodies in the blood sample, how many, and which proteins from the virus they recognised.
Antibodies after vaccination
In the Netherlands, various vaccines are being used to protect people against the coronavirus: RNA vaccines and vector vaccines. Both types of vaccine cause the body to produce antibodies against the virus, but they do so in different ways.
Protection resulting from RNA vaccines
The COVID-19 vaccines made by Pfizer/BioNTech and by Moderna are RNA vaccines. These vaccines contain a code (the mRNA) to make a very small piece of the coronavirus: the spike protein. The cells of your body that take in the code then start producing this spike protein. After that, the immune system recognises the spike proteins as foreign substances and starts making antibodies. Once that happens, if you come into contact with the virus, you will be protected by those antibodies. This minimises the chance that you will become ill from the virus.
Protection resulting from vector vaccines
AstraZeneca and Janssen are vector vaccines. These vaccines use a modified and harmless virus to transport a substance into your body: in this case, a fragment of SARS-CoV-2. This harmless virus is known as a vector. The AstraZeneca vaccine uses the adenovirus as the vector. A vector cannot replicate or make you ill. The fragment of SARS-CoV-2 code that is inside the vector vaccine causes it to make the spike protein. Your body then produces antibodies in response. This is how your defences are developed. Read more about vaccine efficacy and protection.